How Much Does Medicare Pay for Physical Therapy in 2024?
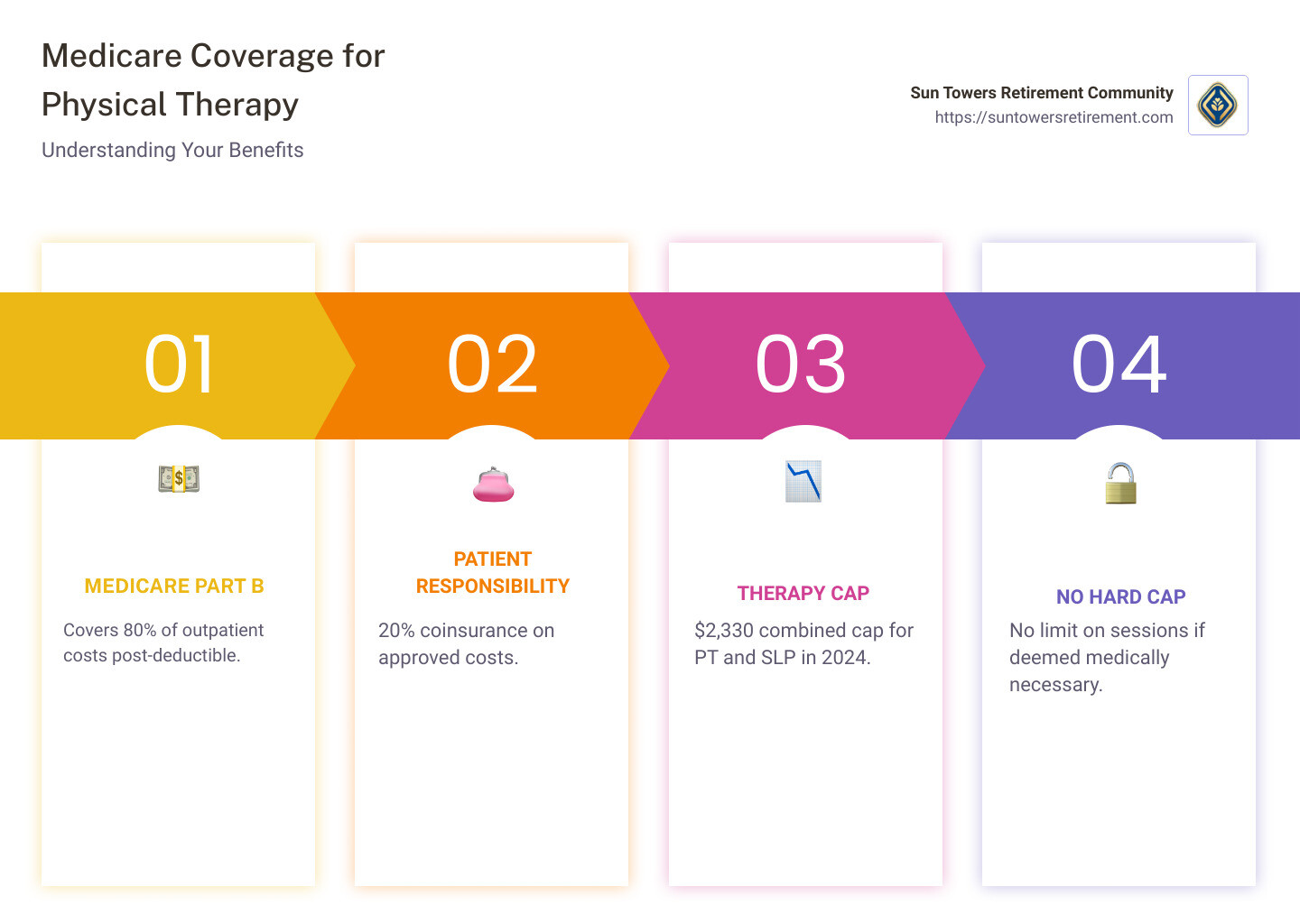
How much does Medicare pay for physical therapy per visit is a common question many seniors ask when considering their healthcare options. Medicare Part B typically covers 80% of approved costs for outpatient physical therapy, with the patient responsible for a 20% coinsurance once their deductible for the year is met.
Navigating healthcare costs can be overwhelming, especially when it comes to understanding how Medicare works for physical therapy. Ensuring you receive the right care without breaking the bank is crucial. Physical therapy is often necessary to improve or maintain physical health, and outpatient therapy services are covered as long as they are deemed medically necessary.
It’s reassuring for many to know that Medicare no longer imposes a hard cap on physical therapy services. That said, there is a combined limit of $2,330 in 2024 for physical therapy and speech-language pathology, after which additional services must be confirmed as necessary by providers.
Understanding Medicare Coverage for Physical Therapy
Medicare coverage for physical therapy can seem complex, but breaking it down helps. Let’s explore how Medicare Part A, Part B, Medicare Advantage, and Medigap play roles in covering these services.
Medicare Part A
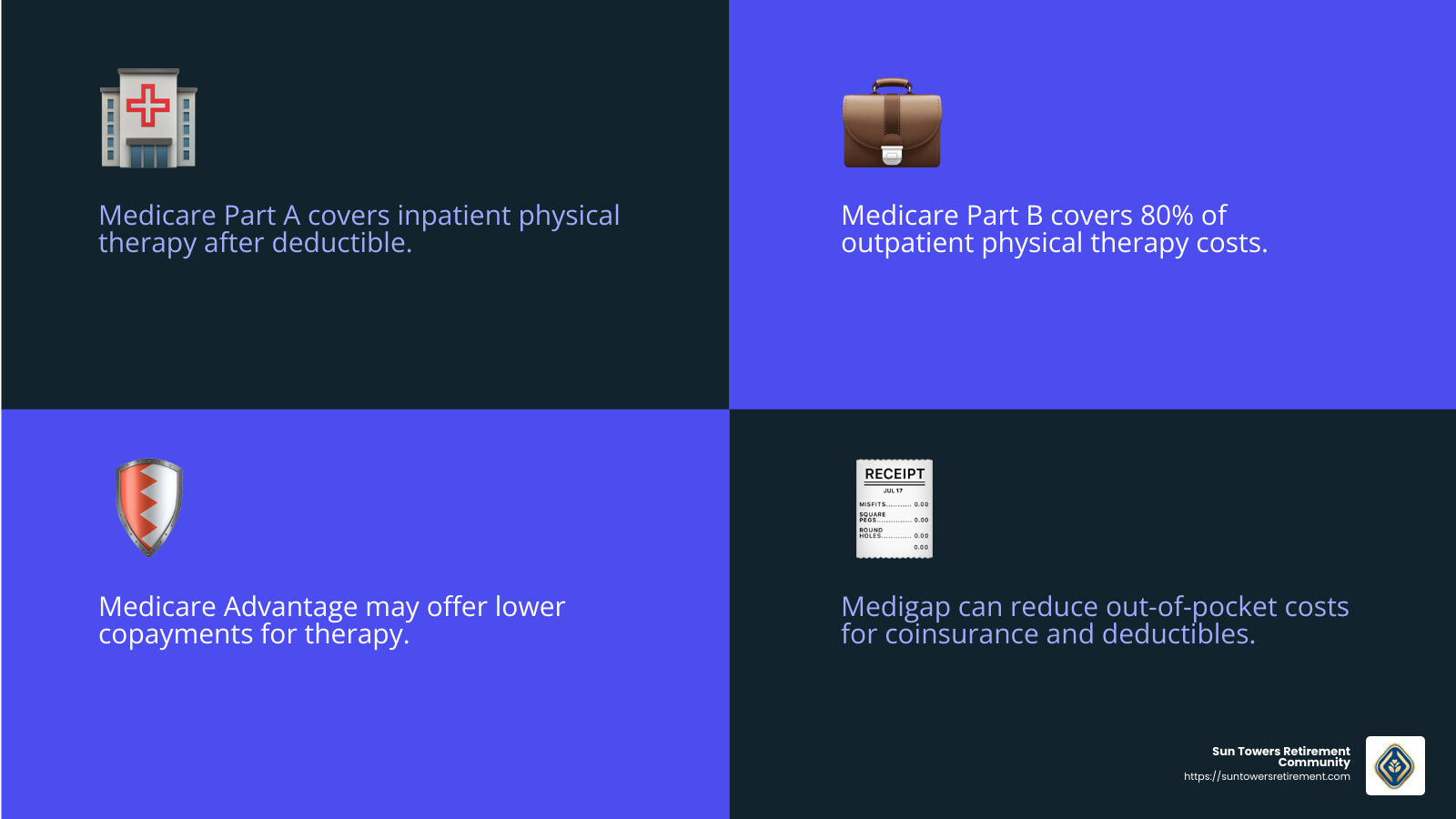
Medicare Part A is often thought of as hospital insurance. It covers inpatient physical therapy for those admitted to a hospital or a skilled nursing facility. This coverage kicks in after you’ve paid your deductible. For example, if you need intensive rehabilitation after surgery, Part A may cover the costs, but approval from your doctor is crucial.
Medicare Part B
When it comes to outpatient physical therapy, Medicare Part B is your go-to. It covers 80% of the Medicare-approved amount once your deductible is met. This means if your therapy costs $100, Medicare pays $80, and you’re responsible for the remaining $20. The therapy must be medically necessary and approved by a healthcare provider.
Medicare Advantage
Medicare Advantage plans, also known as Part C, are offered by private insurance companies. They include all the benefits of Part A and Part B and often offer additional perks. For physical therapy, these plans may provide lower copayments or additional services. However, costs and coverage vary, so review your specific plan details.
Medigap
Medigap, or Medicare Supplement Insurance, helps cover the “gaps” in Original Medicare, such as copayments and deductibles. If you have Medigap, it can significantly reduce your out-of-pocket costs for physical therapy services. For instance, if you have a 20% coinsurance under Part B, Medigap might cover this portion, depending on your plan.
Understanding these components can help you make informed decisions about your physical therapy needs. Each part of Medicare plays a role in ensuring you get the care you require without unexpected expenses.
How Much Does Medicare Pay for Physical Therapy Per Visit?
Factors Affecting Costs
When considering physical therapy under Medicare, it’s important to understand the costs involved. Typically, Medicare Part B covers 80% of the approved cost for outpatient physical therapy. However, several factors influence how much you might pay out of pocket.
Part B Deductible and Coinsurance
Before Medicare Part B starts covering your therapy costs, you need to meet the annual deductible. For 2024, this deductible is $204. Once met, Medicare pays 80% of the therapy costs, leaving you with a 20% coinsurance. So, if a therapy session costs $100, Medicare pays $80, and you are responsible for $20.
Medically Necessary Services
Medicare only covers therapy that is deemed medically necessary. This means your doctor or therapist must certify that the therapy is required to improve or maintain your health condition. If the therapy isn’t considered necessary, you might have to cover the full costs yourself.
Provider Approval
Your therapy must be provided by a Medicare-approved provider. This ensures that the services meet Medicare’s standards and that you receive the coverage you’re entitled to. Always confirm that your therapist is approved to avoid unexpected expenses.
Therapy Setting
Where you receive your therapy can also affect costs. Medicare Part B covers therapy in various settings, including:
- Private offices
- Hospital outpatient departments
- Skilled Nursing Facilities (when Part A isn’t involved)
- Rehabilitation facilities
- At home, if provided by a qualified therapist
Each setting might have different associated costs, so it’s crucial to understand how these settings impact your expenses.
By understanding these factors, you can better steer the costs of physical therapy under Medicare and plan for any out-of-pocket expenses. This knowledge ensures you make the most of your Medicare benefits while managing your healthcare budget effectively.
Inpatient vs. Outpatient Physical Therapy Costs
Understanding the differences between inpatient and outpatient physical therapy costs under Medicare is essential for managing your healthcare expenses effectively.
Inpatient Rehabilitation
When you receive physical therapy in an inpatient rehabilitation facility, Medicare Part A typically covers the costs. This type of therapy is common after a major surgery or severe illness. The costs are bundled into the overall expenses of your hospital or rehab stay.
- Days 1-60: You pay a deductible of $1,556.
- Days 61-90: You pay a daily coinsurance of $389.
- Day 91 and beyond: You have 60 lifetime reserve days with a coinsurance of $778 per day. After these are used, you cover all costs.
Medicare covers your therapy along with other hospital services like room charges and meals.
Skilled Nursing Facilities
In a skilled nursing facility, Medicare covers physical therapy if you meet specific requirements, such as a prior hospital stay of at least three days.
- First 20 days: Medicare covers all costs.
- Days 21-100: You pay a daily coinsurance of $194.50.
- Day 101 and beyond: You are responsible for all costs.
This coverage includes not only therapy but also room and board, nursing care, and other necessary services.
Outpatient Settings
For outpatient physical therapy, Medicare Part B is responsible for coverage. This includes therapy received at:
- Private offices
- Hospital outpatient departments
- Comprehensive Outpatient Rehabilitation Facilities (CORFs)
Medicare pays 80% of the approved amount after you meet the annual deductible ($204 in 2024), leaving you with a 20% coinsurance.
In outpatient settings, therapy must be medically necessary and provided by a Medicare-approved provider to qualify for coverage.
Understanding these differences helps you anticipate costs and make informed decisions about where to receive your therapy based on your financial and medical needs.
This knowledge allows you to maximize your Medicare benefits and manage your healthcare budget effectively.
Maximizing Your Medicare Benefits for Physical Therapy
When it comes to getting the most out of your Medicare benefits for physical therapy, there are a few key points to keep in mind.
No Session Limit
First, the good news: Medicare does not limit the number of physical therapy sessions you can have. As long as the therapy is deemed medically necessary, you can continue receiving treatment. This means you can keep attending sessions until you achieve your health goals, without worrying about hitting a session cap.
Therapy Cap
However, while there is no session limit, there is a therapy cap to be aware of. In 2024, Medicare has set a $2,330 cap for combined physical therapy and speech-language pathology services. Once you reach this limit, your therapist must confirm that further therapy is medically necessary for Medicare to continue covering the costs. This confirmation is done using a special code called the KX Modifier.
Medically Necessary Confirmation
To ensure your therapy is covered, it must be medically necessary. This means a doctor or licensed therapist must document that the therapy is essential for your health. Medicare requires regular evaluations to confirm this necessity, especially if your therapy costs exceed the $2,330 cap. If therapy continues past $3,000, Medicare may conduct a medical review to ensure services are still needed.
By understanding these factors, you can make the most of your Medicare benefits for physical therapy, ensuring you receive the care you need without unnecessary financial stress.
Frequently Asked Questions about Medicare and Physical Therapy
How many PT sessions will Medicare cover?
Medicare does not set a limit on the number of physical therapy sessions you can receive. The key requirement is that the therapy must be medically necessary. This means that as long as your doctor or physical therapist certifies that the therapy is essential for your health, you can continue with as many sessions as you need.
What is the Medicare physical therapy cap for 2024?
In 2024, Medicare has a $2,330 cap for combined physical therapy (PT) and speech-language pathology (SLP) services. This cap is not a hard limit on the number of sessions but rather a threshold for costs. If your therapy expenses exceed this amount, your provider must confirm that further therapy is medically necessary to continue receiving coverage. This is done using a special code known as the KX Modifier.
Can Medicare deny physical therapy coverage?
Yes, Medicare can deny coverage for physical therapy if it’s not deemed medically necessary. For therapy to be covered, a licensed physician or therapist must authorize and document the necessity of the services. Without this authorization, Medicare will not pay for the therapy. Additionally, if your therapy costs exceed $3,000, Medicare may conduct a medical review to ensure that the services are still required for your health.
Conclusion
At Sun Towers Retirement Community, we understand the importance of comprehensive care, especially when it comes to physical therapy. Our goal is to help you or your loved ones maintain mobility and improve quality of life in a supportive environment.
We offer a range of therapy services, including physical, occupational, and speech therapies. Our skilled team uses advanced equipment and personalized care plans to meet the unique needs of each resident. Whether you’re recovering from surgery or managing a chronic condition, our therapy services are designed to help you achieve your health goals.
Physical therapy is an essential part of our continuum of care. We focus on helping residents regain strength, improve balance, and improve overall well-being. Our therapists work closely with doctors to ensure that each therapy session is medically necessary and custom to individual health needs.
For more information on our therapy services and how we can help you make the most of your Medicare benefits, visit our therapy services page. At Sun Towers, we are committed to providing quality care and support every step of the way.